Winnipeg’s Mental Health Landscape: Depression Rates, Statistics, and Impacts
Key Insights
| The University of Manitoba reveals that in 2018, 28% of all adults in the province lived with at least one form of mental illness. A 2019 study on the prevalence of mental disorders and suicidality in Canadian provinces showed that Manitoba had the highest rate of adults reporting any mental disorder, at 13.63%. The same study also found that around 7.01% of adults reported having a major depressive disorder. Statistics Canada illustrates that around 60.1% of adults in Manitoba rated their overall mental health as very good or excellent. According to data from the National Library of Medicine, the average direct medical cost for individuals with depression amounted to around $10,064 per year. |
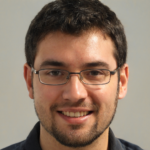
According to a 2018 study by the University of Manitoba, 28% of adults in the province are living with at least one mental illness.
This means that mental illness affects more than one in four adults in Manitoba, and thus highlights the growing need to look into this issue.
The data shows that mood and anxiety disorders are the most commonly experienced illnesses, affecting 23% of adults. These conditions include depression, generalized anxiety disorder, panic disorder, and related diagnoses.
Individuals with mood and anxiety disorders often experience symptoms that interfere with daily activities, productivity, and social relationships.
Meanwhile, addictions affect 6% of the adult population. This category includes dependency on alcohol, prescription medications, and illicit substances, along with behavioral addictions such as gambling.
On the lower end of the list, psychotic disorders affect 2% of adults. These include conditions characterized by delusions, hallucinations, or disorganized thinking, which can severely disrupt a person’s ability to function.
Although psychotic disorders are less common than mood or anxiety conditions, they require intensive, long-term psychiatric care and support systems.
Schizophrenia accounts for 1% of all cases. This chronic mental illness often involves long-term symptoms such as auditory hallucinations, impaired cognition, and isolation.
Similarly, personality disorders also affect 1% of the adult population. These conditions are marked by patterns of thought and behavior that cause significant distress or difficulty in relationships.
Individuals with personality disorders may require long-term psychotherapy and community-based support, but are often underdiagnosed due to overlapping symptoms with other conditions.
Overall, the data gives an overview of the mental health landscape in the region and points to which issues need the most attention.
| Mental Illness Category | Percentage of Adults Affected |
| Mood and Anxiety | 23% |
| Addictions | 6% |
| Psychotic Disorders | 2% |
| Schizophrenia | 1% |
| Personality Disorders | 1% |
| Total percentage of adults in Manitoba with at least 1 mental illness | 28% |
Regional Analysis of Mental Illness Rates Across Canada
According to a study on the prevalence of mental disorders and suicidality in Canadian Provinces in 2019, there was a total of 13.63% of adults in Manitoba who reported having any mental disorder.
This is the highest rate recorded among all Canadian provinces. It is notably higher than the national average of 9.59% and reflects a much heavier mental health burden in the province.
Nova Scotia follows with a rate of 12.51%, while Saskatchewan, Alberta, and British Columbia all report rates just above 10%.
In contrast, Prince Edward Island reports the lowest rate in the country at 7.66%, showing a gap of nearly 6 percentage points between the highest and lowest provinces.
Meanwhile, major depressive disorder was reported by 7.01% of adults in Manitoba. This is also the highest rate in the country and stands well above the national average of 4.72%.
The next highest rate is in Nova Scotia at 5.60%, while most provinces fall between 4% and 5.5%. Prince Edward Island reports the lowest rate at 2.92%.
Manitoba’s rate is almost double that of the lowest province and indicates that depression is a leading mental health issue in the region.
Furthermore, the rate of bipolar disorder in Manitoba is 1.38%. This is slightly below the national rate of 1.51% and places Manitoba in the middle of the national range.
Newfoundland and Labrador reports the highest rate at 1.85%, while Prince Edward Island had the lowest rate at 1.09%.
Generalized anxiety disorder affects 3.51% of Manitoba’s population. This is among the highest rates nationally, exceeded only by Newfoundland and Labrador at 3.70%.
Manitoba’s rate is also significantly higher than the national average of 2.57%, which shows that anxiety-related disorders affect a larger share of people in this region.
Another alarming statistic to note is that alcohol use disorder is reported by 3.38% of Manitoba adults, making it the highest rate in Canada. The national average is 2.22%.
Along with this, substance use disorder also affects 2.34% of the population in Manitoba, making it one of the highest in the country. Only Nova Scotia, at 2.89%, reports a higher percentage.
The data suggests that a substantial number of Manitobans are affected by issues involving drugs or other substances that interfere with daily functioning.
As for other issues, suicidal ideation is reported by 5.12% of adults in Manitoba. This is the highest rate in the country and far exceeds the national average of 3.34%.
There is also a considerable gap between Manitoba and the second-highest province, Nova Scotia, which is a whole percentage point lower at 4.12%.
Related to this, suicidal plans were reported by 1.42% of Manitoba adults. This rate is higher than the national figure of 1.14% and is again the highest rate in the country.
Manitoba’s figure suggests a larger proportion of individuals are progressing beyond ideation to a more serious mental health risk.
As for actual suicide attempts, this was reported by 0.46% of adults in Manitoba, which is below the national average of 0.53%.
While the data shows that there is a lower percentage of adults who attempt suicide in Manitoba, it is still alarming that the province ranked first for suicidal ideation and suicidal plans.
The province also ranks first for the categories of number of residents with any mental disorder, major depressive disorder, and alcohol use disorder. Manitoba also had among the highest rates in other categories.
Thus, these numbers show the relatively poorer state of mental health in Manitoba, in relation to other provinces. This also highlights what disorders are the most prevalent in the region.
| Category | Canada | BC | AB | SK | MB | ON | QC | NB | PEI | NS | NFLD |
| Any mental disorder | 9.59 | 10.08 | 10.41 | 10.51 | 13.63 | 9.17 | 8.54 | 10.91 | 7.66 | 12.51 | 9.02 |
| Major depressive disorder | 4.72 | 4.62 | 4.54 | 3.74 | 7.01 | 4.85 | 4.41 | 4.57 | 2.96 | 5.60 | 4.50 |
| Bipolar disorder | 1.51 | 1.42 | 1.66 | 1.32 | 1.38 | 1.76 | 1.10 | 1.47 | 1.09 | 1.48 | 1.85 |
| Generalized anxiety disorder | 2.57 | 2.63 | 2.48 | 3.18 | 3.51 | 2.52 | 2.25 | 3.41 | 2.33 | 3.09 | 3.70 |
| Alcohol use disorder | 2.22 | 2.59 | 2.69 | 2.59 | 3.38 | 1.87 | 2.11 | 2.46 | 2.10 | 2.29 | 1.63 |
| Substance use disorder | 1.78 | 1.77 | 1.82 | 2.18 | 2.34 | 1.68 | 1.71 | 1.85 | 0.95 | 2.89 | 1.27 |
| Suicidal ideation | 3.34 | 3.42 | 2.99 | 3.88 | 5.12 | 3.60 | 2.74 | 2.95 | 2.22 | 4.12 | 2.34 |
| Suicidal plans | 1.14 | 1.38 | 0.90 | 0.64 | 1.42 | 1.28 | 1.04 | 0.63 | 0.80 | 0.73 | 0.49 |
| Suicide attempt(s) | 0.53 | 0.53 | 0.27 | 0.57 | 0.46 | 0.69 | 0.41 | 0.34 | 0.25 | 0.43 | 0.40 |

Mental Health Trends in Winnipeg
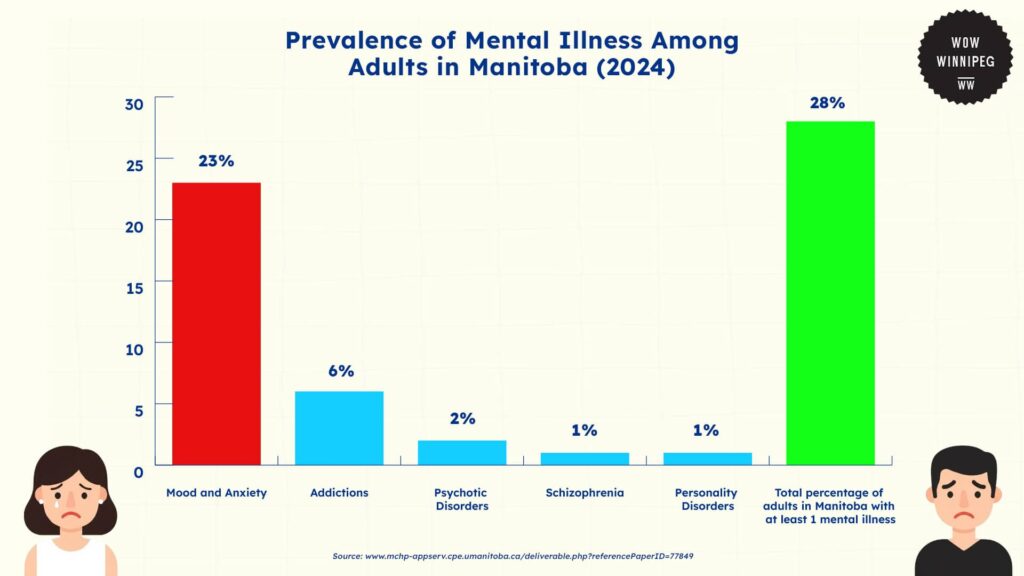
Despite having the highest rate of diagnosed mental disorders in the country, Statistics Canada reveals that 60.1% of adults in Manitoba rate their overall health as very good or excellent.
This figure is close to the national average of 60.8%, suggesting that general health perception in the province is aligned with trends across Canada.
Similarly, 68.1% of Manitobans report very good or excellent mental health. This is also close to the national average of 69.4%, despite Manitoba’s higher diagnosed mental illness rates.
When asked about stress levels, 18.8% of Manitobans said they experience quite a bit or extreme life stress.
This is slightly below the national figure of 21.4%, suggesting that while many face mental health concerns, overall perceived stress is not exceptionally high in the province.
Mood disorders, which include depression, bipolar disorder, mania, or dysthymia, are self-reported by 9.9% of Manitobans. This is just above the national average of 8.8%, and aligns more closely with diagnosis rates in the province.
Heavy drinking is reported by 16.3% of Manitobans, which is slightly higher than the national average of 19.3%. Meanwhile, the smoking rate in the province is 16.7%, aligning closely with the national rate of 16.0%.
These trends also align with statistics on addiction in the province, particularly for alcohol abuse.
As for how well the province deals with these issues, healthcare access in Manitoba is perceived to be generally strong. A total of 83.9% of residents report having a regular healthcare provider, which is slightly below the national figure of 84.9%.
Plus, a sense of belonging to the local community is reported by 73.6% of Manitobans, higher than the national average of 68.9%. This suggests that community connection may be another positive factor for well-being in the province.
Finally, personal satisfaction in Manitoba also seems to be strong. A total of 93.2% of adults reported being satisfied or very satisfied with life, which is very close to the country average of 93.1%.
Together, these indicators suggest that Manitoba’s population reports average or above-average levels of satisfaction, access to care, and community connection, despite elevated rates of diagnosed mental health conditions.
Since these may paint a mixed picture of mental health in the region, they also indicate a need to look into self-reporting and understanding of mental health in the province.
| Indicator | Manitoba | Canada |
| Very good or excellent health | 60.1 | 60.8 |
| Very good or excellent mental health | 68.1 | 69.4 |
| Life stress (quite a bit or extremely stressful) | 18.8 | 21.4 |
| Mood disorder (self-reported) | 9.9 | 8.8 |
| Heavy drinking (adult) | 16.3 | 19.3 |
| Smoking (daily or occasional, adult) | 16.7 | 16.0 |
| Has a regular healthcare provider | 83.9 | 84.9 |
| Life satisfaction (satisfied or very satisfied) | 93.2 | 93.1 |
| Sense of community belonging (strong or somewhat strong) | 73.6 | 68.9 |
Costs and Consequences of Rising Mental Illness Trends in Winnipeg
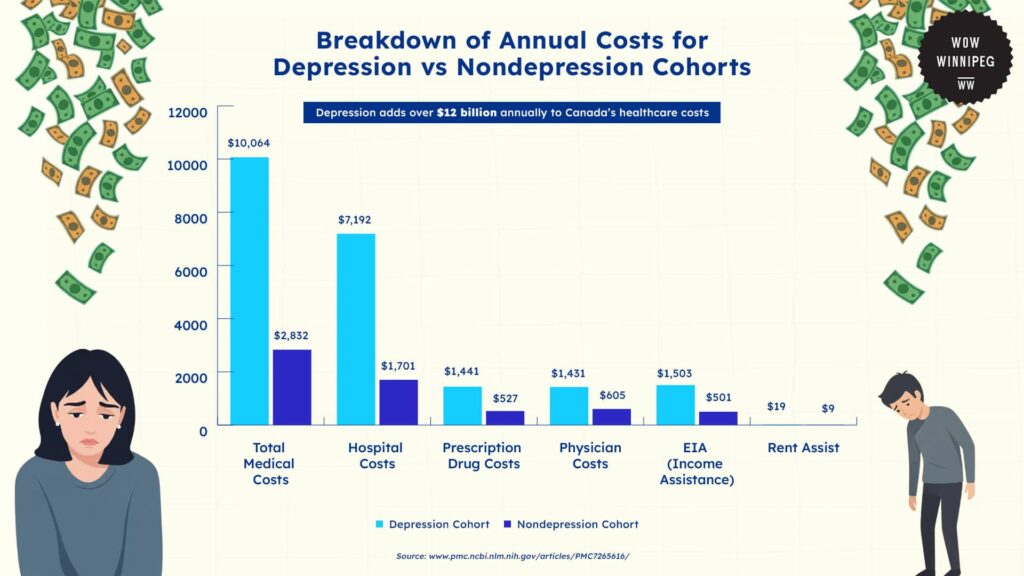
A study by the National Library of Medicine found that mental illness and depression cause significant financial burdens for both diagnosed individuals and the broader society.
In a cohort study involving residents from Manitoba, patients diagnosed with depression had health care costs that were more than 3.5 times higher than those without depression.
The average direct medical cost per person with depression was $10,064 per year, compared to $2,832 for individuals without depression.
This figure includes hospitalizations, physician visits, prescription medications, and psychotherapy. These differences reflect the higher healthcare demand and frequency of service use associated with mental illness.
Hospital costs were the largest contributor to this large gap in costs. Among patients with depression, average annual hospital-related expenses reached $7,192, while those without depression averaged only $1,701.
Prescription drug costs followed a similar pattern. Depressed individuals incurred average medication expenses of $1,441 per year, which is nearly three times more than the $527 reported by nondepressed individuals.
As for physician services, patients with depression incur an average of $1,431 in annual costs, which is more than double the $605 average for those without depression.
Beyond these direct costs, the burden caused by mental illness also extends into social service programs. Depression is linked to higher use of public supports, including Employment and Income Assistance (EIA) and rent assistance.
Average EIA costs for individuals with depression totaled $1,503 per year, compared to $501 for those without depression. Rent assist costs were also higher, at $19 for patients with depression versus $9 for others.
On a larger scale, the financial impact of depression is also substantial. In Manitoba alone, depression is projected to cost the provincial healthcare and social service systems an additional $400 million annually.
When these findings are expanded to the national level, the estimated cost to the Canadian healthcare system exceeds $12 billion per year.
These figures represent only direct system costs and do not account for indirect economic losses due to reduced workforce participation, lost productivity, and the burden placed on family members or caregivers.
Overall, these numbers reveal how those experiencing depression are financially disadvantaged in society, while also showing how these costs affect the broader economy as a whole.
| Cost Category | Depression Cohort | Nondepression Cohort |
| Total Medical Costs | $10,064 | $2,832 |
| Hospital Costs | $7,192 | $1,701 |
| Prescription Drug Costs | $1,441 | $527 |
| Physician Costs | $1,431 | $605 |
| EIA (Income Assistance) | $1,503 | $501 |
| Rent Assist | $19 | $9 |
Interventions and Solutions to Rising Mental Illness Trends in Winnipeg
The Winnipeg Regional Health Authority (WRHA) delivers a wide range of community-based mental health services aimed at supporting individuals across the spectrum of mental health needs.
These services are designed to be accessible and recovery-oriented, with a strong focus on helping individuals live independently and remain integrated in their communities.
One of the core services offered is mental health assessment and counseling. Individuals can access support for crisis intervention, short-term therapy, and referrals to additional resources.
For those with ongoing needs, WRHA also offers community mental health case management.
This involves working with a community mental health worker who assists in developing a personalized care plan, coordinates access to services, and provides consistent support over time.
Rehabilitation and education programs are another key component in this program. These initiatives focus on helping individuals build daily living skills, regain confidence, and pursue education or employment.
Complementing this are housing support services, which help individuals locate, choose, and maintain appropriate housing, which is an essential foundation for mental stability and long-term recovery.
The WRHA also provides proctor support services. These are designed to assist individuals in developing independent living skills and help them attend medical appointments or manage daily tasks.
This type of support is particularly valuable for clients transitioning out of a hospital setting or those with complex needs.
In addition to its core services, WRHA works in close collaboration with multiple community agencies to extend its reach.
Organizations such as Klinic Community Health and the Canadian Mental Health Association (CMHA) Manitoba and Winnipeg contribute additional support in areas such as creative expression, peer support, employment services, and specialized counseling.
These partnerships create a broader system of care that enables individuals to access services aligned with their goals, culture, and circumstances.
Altogether, this community-based approach allows for continued care for patients, from crisis response to long-term rehabilitation. These reduce reliance on inpatient services and improve the quality of life for individuals with mental health conditions in Manitoba.
The Future of Depression and Mental Health Trends in Winnipeg
Based on current trends, Winnipeg is expected to face continued strain on its mental health system in the coming years.
With 13.63% of adults in Manitoba already reporting a mental disorder, which is a higher rate than any other province in the country, the demand for mental health services is unlikely to slow down.
Moreover, if rates of major depressive disorder and suicidal ideation remain high, Winnipeg will need to prepare for increasing pressure on hospitals, community mental health programs, and social services.
Without increased access to early intervention and long-term community support, individuals will continue to be financially burdened, and the economic impact on the city could surpass the current projection of $400 million annually.
On a more positive note, Manitoba’s strong self-reported sense of community belonging and high life satisfaction do offer opportunities for improvements in mental health services
If WRHA’s community-based mental health services continue to expand, the city could shift toward more preventative and recovery-oriented care.
With continued investment, Winnipeg has the potential to reduce reliance on crisis services and improve long-term outcomes for the city, which can then decrease mental illness diagnoses in the city.
References
- Chartier, M., Brownell, M., MacWilliam, L., Valdivia, J., Nie, Y., & Ekuma, O. (2019). The cost of mental health services use in Manitoba: A population-based study. Manitoba Centre for Health Policy. http://mchp-appserv.cpe.umanitoba.ca/deliverable.php?referencePaperID=77849
- Katz, A., Chateau, D., Enns, J., & Sareen, J. (2019). Association of depression with 10-year mortality among community-dwelling adults in Canada: A population-based cohort study. The Canadian Journal of Psychiatry, 64(12), 845–852. https://doi.org/10.1177/0706743719878987
- Statistics Canada. (2019). Perceived mental health, 2015 to 2018. https://www150.statcan.gc.ca/n1/pub/82-625-x/2019001/article/00014/cma-rmr27-eng.htm
- Vigo, D., Jones, W., & Thornicroft, G. (2020). Burden of mental, neurological, substance use disorders and self-harm in Canada, 1990–2017: A Canadian perspective on global burden of disease data. Canadian Journal of Psychiatry, 65(10), 712–720. https://pmc.ncbi.nlm.nih.gov/articles/PMC7265616/
- Winnipeg Regional Health Authority. (n.d.). Community mental health services. https://wrha.mb.ca/mental-health/community-mental-health-services/
- Enns, J., Chateau, D., Metge, C., Dulai, J., & Katz, A. (2019). Does having a regular primary care provider reduce the likelihood of hospital admissions and emergency department visits? Canadian Family Physician, 65(10), e450–e456. https://pubmed.ncbi.nlm.nih.gov/31619055/
- Statista. (2021). Share of Canadians reporting high depression symptoms before and since COVID-19 pandemic as of May 2021. https://www.statista.com/statistics/1221071/high-depression-before-since-covid-pandemic-canada/
- Canadian Mental Health Association. (2024). State of mental health profile: Manitoba. https://cmha.ca/wp-content/uploads/2024/11/State-of-Mental-Health-profile-Manitoba.pdf
- Government of Manitoba. (2021). Annual statistics 2021: Manitoba Health. https://www.gov.mb.ca/health/annstats/as2021.pdf